The eLitMed.hu medical portal uses computer cookies for convenient operation. Detailed information can be found in the Cookie-policy.
Hypertension and nephrology - 2020;24(03)
Content
[Treatment of hypertension in patients with chronic renal failure]
[The prevalence of chronic renal failure and hypertension is steadily increasing worldwide. The risk of possible cardiovascular death in patient with advanced renal failure is greater than the risk of progression to end-stage renal failure. Therefore treating and achieving target blood pressure is important in order to slow renal function decline in parallel with cardiovascular risk reduction. However, guidelines do not specify a single blood pressure target to be achieved in patients with renal failure, but suggest evidence based, reno- and cardioprotective therapy. This paper summarizes the clinical practice of treating hypertension (drug and nondrug treatment, therapeutic algorithm, target value, effectiveness of therapy) in patients with chronic renal failure.]
[Covid-19 and the kidney]
[Covid-19 pandemy has emerged from Wuhan, China in December 2019. The infection affects not only the lung but other organs such as the kidney, as well. The relation between Covid-19 infection and the kidney is bidirectional. On one hand, Covid-19 infection may cause kidney damage in 50-75% of the cases resulting in proteinuria, haematuria and acute kidney injury (AKI). The etiology of AKI is multifactorial. Main pathogenic mechanisms are direct proximal tubular cell damage, sepsis-related haemodinamic derangement, citokine storm and hypercoagulability. The virus enters proximal tubular cells and podocytes via the ACE2 receptor followed by multiplication in the lysomes and consequential cell lesion. Histopathology shows acute tubular necrosis and acute tubulointerstitial nephritis. AKI is a strong predictor of mortality in critically ill patients. On the other hand, the risk of Covid-19 infection and mortality is substantially increased in patients with chronic kidney disease – especially in those with a kidney transplant or on dialysis – due to their immunocompromised status. Among haemodialysis patients, infection may spread very easily due to the possibility of getting contacted in the ambulance car or at the dialysis unit. The mortality rate of patients on renal replacement therapy with Covid-19 infection is 20-35%. In order to avoid mass infection it is obligatory to employ preventive measures and implement restricions along with (cohors) isolation of infected patients. In Hungary, every dialysis or kidney transplant patient with Covid-19 infection should be admitted to dedicated Covid-19 wards.]
[Hypertension and Covid-19 – Part I. Significance of age, underlying diseases, and ACEI/ARB therapy in hypertension and co-morbidities during SARS-Cov2 infection]
[The appearance of the Covid-19 epidemic in different continents shows specific clinical features. Confirmed infected patients are detectable from approximately 30 years, with a maximum between 40 and 70 years of age. At the same time, however, a significant proportion of those who die from the infection come from patients over 65 years. The prevalence and mortality rates of the hypertensive population show a very similar formation. Based on the data collected, it is not surprising that hypertension as the underlying disease in the Covid- 19 epidemic is the first in all analysis. A more precise analysis clarified that it is not hypertension per se, but co-morbidities and complications of hypertension that play a primary role behind large-scale mortality in old age, such as diabetes, coronary heart disease, stroke, heart failure, and chronic kidney disease. Data from China, North America, and Italy suggest that hypertension and diabetes – and in North America, pathological obesity – in infected patients actually only reflect the prevalence of these diseases in a given population. The presence of comorbidities (coronary artery disease, stroke, heart failure, arrhythmia, chronic kidney disease) – based on multivariate logistic regression analysis – presents a more risk for severe clinical course and mortality. Some recent analyses have provided strong evidence that ACEI/ARB treatment does not pose a higher risk for the course or outcome of infection. Their administration is constantly needed in hypertension and comorbidities due to their organ protective and slowing the progression of diseases.]
[Not all young, athletic university students have optimal blood pressure. Results of the May 2019 Measurement Month (MMM19)]
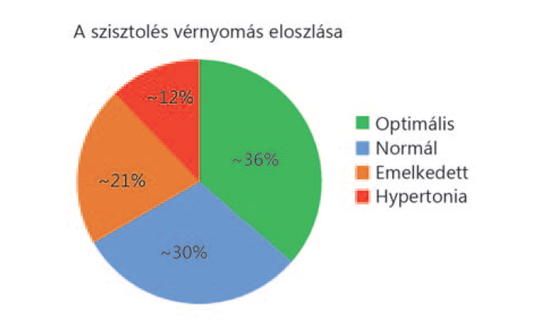
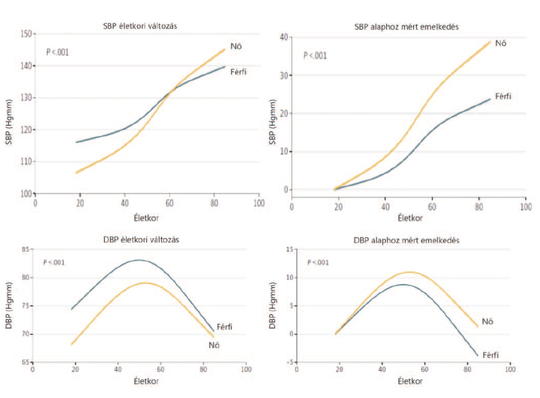
[For about 100 years, it has been known that persistently high blood pressure (hypertension) is the leading cause of cardiovascular disease deaths, such as major risk factors for heart failure, myocardial infarction, stroke, kidney and eye disease. Unfortunately, one of the characteristics of hypertension is that it remains undetected for a long time until damage to one or more organs has already occurred. Therefore, it is very important that systemic blood pressure is monitored from time to time, especially above 45 years of age. The prevalence of hypertension is more than 35% in the Hungarian population. Recent data have pointed out that hypertension may occur at a younger age, although at a lower frequency. Our studies were conducted in the context of the May 2019 Measurement Month (MMM19), an international campaign that draws attention to hypertension and the lack of systematic screening at population level. We hypothesized that hypertension may occur in young, apparently healthy university students. The studies were conducted among students of the University of Physical Education (n = 33; 25 males, 8 females). The mean age was 24.3 years (20–34 years). To measure blood pressure, an automatic blood pressure monitor (Omron MIT5) was used, placed on individuals’ upper arms, as specified in the guidelines, in a relaxed, sitting position. The measurements were repeated three times at one-minute intervals and the average of the three measurements was statistically analyzed. Blood pressure values (mean ± SEM, averaged over 3 measurements) in the student population were systolic 121.9 ± 14.4 mmHg, diastolic 75.1 ± 9.1 mmHg, mean 90.7 ± 10.9 mmHg, and heart rate: 46.8 ± 5.3 mmHg. Although mean blood pressure was within the normal range, higher values were also found in some individuals. Systolic blood pressure fell by 33% due to elevated normal blood pressure, respectively of Grade 1 hypertension. These data confirmed our hypothesis that hypertension may occur at a young age, despite the fact that members of the study population exercise regularly, which is an important preventive factor in the development of cardiovascular disease. These results underscore the importance of regular blood pressure measurement in adolescents, which may reduce the global spread of hypertension and prevent the development of a number of cardiovascular diseases, including stroke, heart attack, renal failure and mental decline.]
[Systolic and diastolic blood pressure by height, BMI, gender and age between 14 and 18 years of age]
[The aim of the screening program was to investigate blood pressure levels in different ages according to obesity. Blood pressure, heart rate, body composition, bodyweight, height and BMI were assessed. 2202 adolescent (1326 girls, 876 boys) participated in the screening program. The mean systolic blood pressure of all screened adolescents was 126.34 ± 12.55 mmHg. Boy/girl values were 131.87 ± 13.59/117.49 ± 5.69 mmHg, p < 0.001. The mean diastolic blood pressure of all screened adolescents was 71.86 ± 8.74 mmHg. Boy/girl values were 72.61 ± 9.17/66.69 ± 5.04 mmHg, p < 0.001. The 50%, 90%, 95%, and 99% thresholds and cases for systolic, diastolic blood pressure, and the BMI and BodyFluid thresholds, detailed for 14–18 year olds, girls and boys, are tabulated. Systolic blood pressure (SBP) was over 99% in 12 girls (14- year-olds), 39 (15), 42 (16), 33 (17), 5 (18) to height. SBP was over 99% in 17 boys (14-year-olds), 73 (15), 100 (16), 33 (17), 5 (18) to height. It is emphasized that systolic blood pressure (SBP) is > 99% in 12 girls (14 years), 39 (15), 42 (16), 33 (17), 5 (18) to body height. SBP > 99% for 17 boys (14 years), 73 (15), 100 (16), 33 (17), 5 (18) to body height. Elevated diastolic values were associated with elevated systolic values, but less occurred. The percentage of high blood pressure was more frequent among boys and girls who were in the overweight group (58.6% and 18.6%). Normal blood pressure is higher in overweight and obese adolescents and is a significant risk factor for developing high blood pressure in young adulthood.]
[Comparison of kidney transplant patients with IR-tacrolimus and LCP-tacrolimus]
[Tremor is the most common adverse event of tacrolimus, and it correlates with the peak concentration of the drug. LCP-tacrolimus is a prolonged release formulation of tacrolimus to be administered once daily and has a dec - reased Cmax value. Hand tremors are evaluated by the Fahn-Tolosa-Marin (FTM) scale used by the neurologists. In case of hand tremor, tacrolimus is switched to LCP-tacrolimus. Tremor improved significantly in accordance with the STRATO cli - ni cal study, which confirmed that switching to LCP-tacrolimus resulted in clinically significant improvement in hand tremor.]
1.
Clinical Neuroscience
[Headache registry in Szeged: Experiences regarding to migraine patients]2.
Clinical Neuroscience
[The new target population of stroke awareness campaign: Kindergarten students ]3.
Clinical Neuroscience
Is there any difference in mortality rates of atrial fibrillation detected before or after ischemic stroke?4.
Clinical Neuroscience
Factors influencing the level of stigma in Parkinson’s disease in western Turkey5.
Clinical Neuroscience
[The effects of demographic and clinical factors on the severity of poststroke aphasia]1.
2.
3.
4.
5.